Eye Surgery
-
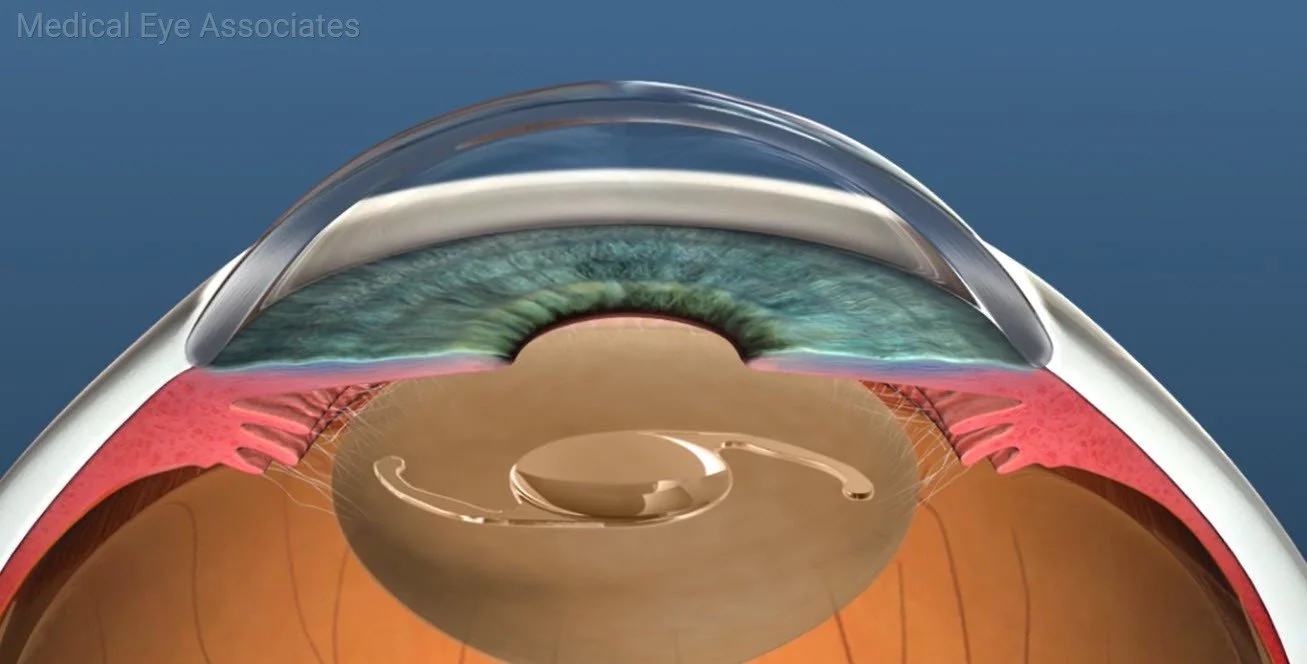
When cataracts start to affect your vision and activities of daily living, they are removed with cataract surgery. Cataract surgery is a minimally invasive surgery and is one of the most common surgeries performed in the United States. During surgery, Dr. Szymarek will remove the cloudy lens (cataract) and replace it with an intraocular lens implant. This implant is very safe for the eye and will last for the rest of your life. The surgery can often be performed without the need for numbing injections or sutures. The surgery is performed at an outpatient surgery center allowing you to return home the same day. You will need to return to see your surgeon the day after surgery for a quick post-operative visit. You will need a driver the day of and the day after surgery. Your surgeon will recommend activity restrictions and eye drops for a few weeks after surgery. Your vision may be blurry the day after surgery and then heal over the next week or two. This is one of the reasons surgery is recommended only on one eye at a time.
The technology of cataract surgery and lens implantation has significantly advanced in recent decades allowing many options for patients. During cataract surgery, your cataract is removed and is replaced with an intraocular lens implant. It is possible to use specialty intraocular lenses to diminish your reliance on glasses after cataract surgery.
MONOFOCAL LENS
If you are happy wearing glasses and hope to continue to wear bifocals, the monofocal lens would be a good option for you. The goal for this lens is to clear your vision. You will still be reliant on glasses for the best focus for some or all activities after the surgery.
SPECIALTY LENSESFor those who aim to be less reliant on glasses after surgery, specialty lenses may be an option for you. Specialty lenses are used to try to place your glasses prescription into the intraocular lens that replaces your cataract after surgery. There are a vast array of specialty lenses, but they can be broken down into two main categories: Toric lenses and Extended Depth of Focus lenses.
TORIC LENS
Toric lenses are used for individuals who have astigmatism. Astigmatism is a condition where your eye is more football shaped than it is round. Glasses are required to correct astigmatism and give your best possible vision. Toric intraocular lenses will place some of your astigmatism correction in your lens implant so that you can have better focus without glasses.
EXTENDED DEPTH OF FOCUS LENSES
Extended depth of focus (EDOF) lenses are a new advanced technology that focuses your vision for both distance and near, minimizing your need for both distance and near glasses after cataract surgery. Not everyone is a candidate for these lenses, and they can carry a slightly increased risk of post-operative glare and halo. Dr. Szymarek will work with you to determine the best possible lens implant for you and your lifestyle needs.
-
The cornea is the clear, dome-shaped front surface of the eye. It plays a crucial role in focusing light entering the eye onto the retina and facilitating clear vision.
There are a number of conditions that can affect the corneal surface, such as recurrent corneal erosions (RCE), corneal dystrophies, corneal scars, and pterygium.
Superficial keratectomy
This is an in-office surgical procedure to help clear the surface of the eye. It involves the removal of the outer layers of the cornea. Utilizing specialized instruments, Dr. Szymarek carefully removes the targeted superficial layers of the cornea. After the removal of the affected tissue, Dr. Szymarek may smooth and shape the corneal surface to optimize its clarity and functionality. Postoperative medications such as antibiotics or anti-inflammatory eye drops are prescribed to aid in healing and prevent infection. Sometimes a bandage contact lens or an amniotic membrane graft is placed on the eye to facilitate healing.
Pterygium excision
A pterygium is a growth of pink, fleshy tissue that can extend onto the cornea. While it is usually benign, a pterygium can occasionally cause discomfort and affect vision if it grows large enough.
Pterygium excision is a surgical procedure performed in the operating room to remove the pterygium from the surface of the eye. The procedure is indicated if the pterygium is causing irregular astigmatism, decreased vision, or significant irritation or discomfort of the eye.
-
Dr. Szymarek is trained in the removal of eyelid lesions, excision of chalazions, and blepharoplasty, which is the removal of excess upper eyelid skin that may droop down and interfere with your vision.
-
Dr. Szymarek is a Fellowship Trained Glaucoma Specialist and Surgeon skilled in managing glaucoma both medically and surgically.
Glaucoma surgery refers to various surgical procedures performed to treat glaucoma, a group of eye conditions characterized by increased intraocular pressure (IOP) that can lead to optic nerve damage and vision loss. The primary goal of glaucoma surgery is to reduce intraocular pressure and preserve the patient's vision.
The choice of glaucoma surgery depends on various factors, including the type and severity of glaucoma, the patient's overall health, and the surgeon's expertise. It is important to note that not all individuals with glaucoma require surgery, and many cases are initially managed with medications or laser treatments. Surgical interventions are typically considered when other treatments are insufficient in controlling intraocular pressure or when there is a significant risk of progression to vision loss.
Here are brief descriptions of some common types of glaucoma surgery:
Tube Shunt Surgery (Glaucoma Drainage Devices):
A small tube or shunt is implanted into the eye to facilitate drainage of aqueous humor, reducing intraocular pressure. The tube is connected to a reservoir (plate) that is placed on the surface of the eye.
Trabeculectomy:
Trabeculectomy involves creating a new drainage channel in the eye to allow excess fluid to drain out, reducing intraocular pressure. A small flap is made in the sclera (the white part of the eye) to create a drainage hole. This creates a filtering bleb which lowers the intraocular pressure in the eye.
Minimally Invasive Glaucoma Surgery (MIGS):
MIGS encompasses a range of newer, less invasive surgical techniques that aim to reduce intraocular pressure with minimal trauma to the eye. The procedures are often performed in conjunction with cataract surgery. Examples include trabecular micro-bypass stents, which create a bypass for aqueous humor to flow out of the eye, and goniotomy and Omni which surgically open up the trabecular meshwork.
Cyclophotocoagulation:
Cyclophotocoagulation involves using laser energy to treat the ciliary body, which produces aqueous humor in the eye. By reducing the production of aqueous humor, intraocular pressure can be lowered.
The choice of glaucoma surgery depends on various factors, including the type and severity of glaucoma, the patient's overall health, and the surgeon's expertise. It is important to note that not all individuals with glaucoma require surgery, and many cases are initially managed with medications or laser treatments. Surgical interventions are typically considered when other treatments are insufficient in controlling intraocular pressure or when there is a significant risk of progression to vision loss.
-
Selective Laser Trabeculoplasty (SLT):
This laser procedure aims to improve the outflow of aqueous humor by treating the trabecular meshwork. SLT is used to treat open-angle glaucoma. It is performed in the office and is safe, painless, and non-invasive. Several clinical trials have demonstrated the safety and efficacy of SLT as a first-line glaucoma treatment.
How does SLT work?
The laser energy stimulates the cells in the drain of the eye, the trabecular meshwork, to function more effectively, which results in greater fluid outflow from the eye. This in turn lowers the pressure inside the eye.
What can I expect during an SLT treatment?
SLT is an outpatient procedure performed in our office. Anesthetic eye drops are used to numb the eye. You will sit at a laser, similar to a slit lamp, and a laser lens is placed on the eye to help focus the laser beam. The application of the laser takes only a few minutes. There is usually no pain during or after the treatment.
What can I expect after SLT treatment?
You may resume normal activities immediately. The eye may be mildly blurry or irritated for a few hours to a day after the procedure. You will use a short course of anti-inflammatory eye drops. A follow-up appointment is usually recommended in about 4 weeks to assess the effect of the laser.
How many treatments are required?
As with any medical procedure, results may vary. Unlike daily eye drops, SLT therapy is administered in a single session in a simple, fast, in-office procedure. Because glaucoma is a chronic disease, follow-up appointments are important. SLT can be safely repeated in the future if necessary.
Is SLT covered by Medicare?
Yes, SLT is covered by Medicare and most insurance providers, potentially saving you thousands of dollars in prescription medication costs.
What are the side effects with SLT?
Unlike many glaucoma medications, there are no incidences of allergy or systemic side-effects with SLT. Complications are rare, but may include inflammation, a temporary increase in eye pressure, blurred vision, headache, red eye, corneal abrasion, or eye pain.
Will I need to continue using eye drops after SLT treatment?
Sometimes SLT can eliminate the need for one eye drop. It will depend on a case by case basis.
Laser Peripheral Iridotomy (LPI):
LPI is a laser procedure used for treating specific types of glaucoma, such as narrow angle and angle closure glaucoma. It involves creating a small hole in the peripheral iris to improve the flow of aqueous humor.
-
A YAG laser capsulotomy is performed to treat posterior capsule opacification (PCO), a common condition that occurs after cataract surgery. During cataract surgery, the cloudy natural lens is removed and replaced with an artificial intraocular lens (IOL) which is implanted into the native lens capsule to restore vision. However, over time, the residual lens capsule may become cloudy, leading to blurred vision, halos, and other visual disturbances. A YAG laser capsulotomy is used to address this issue. Here's a brief description of the procedure:
1. Preparation: The affected eye is dilated with eye drops, and anesthetic eye drops are used to numb the surface of the eye. The patient is seated at the laser in a similar fashion as when being examined at the slit lamp.
2. YAG Laser Application: Dr. Szymarek uses a YAG laser, which stands for yttrium aluminum garnet, to create an opening in the cloudy posterior capsule. The laser delivers energy pulses to create a small, precise hole in the center of the capsule.
3. Clearing the Visual Path: The created opening allows light to pass through the IOL and reach the retina without obstruction, restoring clear vision. The procedure effectively eliminates the cloudiness caused by PCO.
4. Duration and Non-Invasiveness: YAG laser capsulotomy is a quick and non-invasive procedure performed in the office. It is often completed within a few minutes. It does not require incisions or sutures.
5. Post-procedure: Patients often experience a significant improvement in vision following the procedure, and visual recovery is rapid. You can resume normal activities immediately after the procedure. Some patients may notice floaters in their vision temporarily after the procedure, which typically resolves on its own.